Pathology Museum: At University of Kelaniya
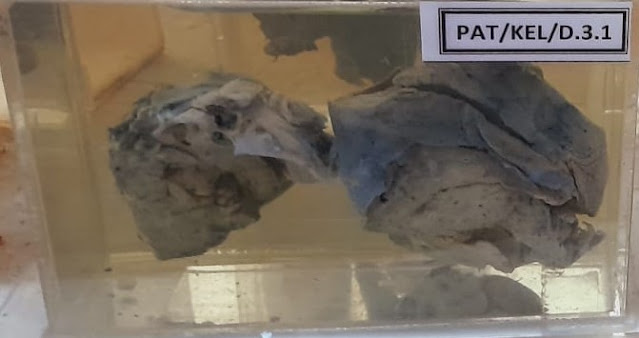
The Brain
01.Purulent meningitis
(Images obtained from the Department of pathology, Faculty of Medicine, University of Kelaniya)
Purulent meningitis is a type of bacterial infection that causes inflammation of the membranes surrounding the brain and spinal cord (meninges).
Cause: Bacterial pathogens, most commonly Streptococcus pneumoniae, Neisseria meningitidis, or Hemophilus influenzae type B, enter the bloodstream and travel to the meninges, leading to infection.
Symptoms: Symptoms typically include severe headache, fever, stiff neck, nausea, vomiting, photophobia (sensitivity to light), altered mental status, and in severe cases, seizures and coma.
Diagnosis: Diagnosis is made through clinical evaluation, lumbar puncture (to examine cerebrospinal fluid for signs of infection), and imaging studies such as CT or MRI scans of the brain.
Treatment: Prompt treatment with intravenous antibiotics (such as ceftriaxone or cefotaxime) is essential to control the infection. Supportive care, including fluid management and medications to reduce fever and alleviate symptoms, is also provided. In some cases, corticosteroids may be used to reduce inflammation. Early diagnosis and treatment are crucial to prevent serious complications and improve outcomes.
02.Pyogenic meningitis
Pyogenic meningitis, also known as bacterial meningitis, is a serious infection of the meninges, the membranes surrounding the brain and spinal cord. Here's a concise overview:
Cause: Bacterial pathogens, such as Streptococcus pneumoniae, Neisseria meningitidis, or Hemophilus influenzae type B, typically enter the bloodstream and spread to the meninges, leading to infection. This can occur through respiratory droplets, close contact with an infected individual, or other means.
Symptoms: Common symptoms include severe headache, fever, neck stiffness, nausea, vomiting, sensitivity to light (photophobia), altered mental status, and in severe cases, seizures or coma. Infants and young children may exhibit irritability, lethargy, poor feeding, and a bulging fontanelle (soft spot on the skull).
Diagnosis: Diagnosis involves a clinical evaluation, including a thorough medical history and physical examination. A lumbar puncture (spinal tap) is performed to collect cerebrospinal fluid (CSF) for analysis, which typically reveals an elevated white blood cell count, increased protein levels, and decreased glucose levels. Imaging studies such as CT or MRI scans may be used to assess for complications.
Treatment: Prompt administration of broad-spectrum antibiotics, such as ceftriaxone or cefotaxime, is crucial to control the infection. Treatment may also include adjunctive therapies such as corticosteroids to reduce inflammation and anticonvulsants for seizure control. Supportive care, including hydration, pain management, and monitoring for complications, is essential. Early recognition and treatment are vital to prevent serious complications and improve outcomes.
03.Prominent vasculature over the surface of the brain
Prominent vasculature over the surface of the brain refers to the visible blood vessels that can be observed on the outer surface of the brain. These blood vessels are part of the cerebral vasculature, which supplies oxygen and nutrients to the brain tissue and removes waste products.
The prominence of these blood vessels can vary depending on factors such as age, health status, and imaging techniques used. In some individuals, particularly infants and young children, the blood vessels may appear more prominent due to thinner skull bones and less fat and connective tissue covering the brain.
In medical imaging studies such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, prominent vasculature may be observed as linear or curvilinear structures on the surface of the brain. This can be a normal variant and typically does not indicate any pathology or abnormality.
However, in some cases, prominent vasculature may be associated with certain medical conditions, such as increased intracranial pressure, vascular malformations, or inflammatory conditions affecting the blood vessels. If prominent vasculature is observed along with other concerning findings or symptoms, further evaluation by a healthcare professional may be warranted to determine the underlying cause.
04.Brain and meninges: subarachnoid hemorrhage
Subarachnoid hemorrhage (SAH) is a medical emergency characterized by bleeding into the space between the arachnoid mater and the pia mater, the two innermost layers covering the brain.
Cause: The most common cause of subarachnoid hemorrhage is the rupture of a cerebral aneurysm, which is a weak spot or bulge in a blood vessel wall. Other potential causes include arteriovenous malformations (AVMs), head trauma, bleeding disorders, or less commonly, infections or tumors.
Symptoms: The hallmark symptom of subarachnoid hemorrhage is a sudden, severe headache, often described as the worst headache of one's life. Other common symptoms include nausea, vomiting, neck stiffness, photophobia (sensitivity to light), altered mental status, and focal neurological deficits such as weakness or numbness. Loss of consciousness or coma may occur in severe cases.
Diagnosis: Diagnosis is typically made through a combination of clinical evaluation, imaging studies, and cerebrospinal fluid (CSF) analysis. Imaging tests such as computed tomography (CT) scans or magnetic resonance imaging (MRI) may show evidence of bleeding in the subarachnoid space. A lumbar puncture (spinal tap) may be performed to analyze CSF for signs of blood and to assess for elevated intracranial pressure.
Treatment: Treatment of subarachnoid hemorrhage aims to control bleeding, prevent complications, and manage symptoms. This may include hospitalization in a specialized stroke or neurocritical care unit. Management may involve blood pressure control, administration of medications to prevent vasospasm (a potentially dangerous narrowing of blood vessels), and supportive care to manage symptoms such as pain, nausea, and seizures. In cases where the hemorrhage is caused by a ruptured aneurysm, surgical or endovascular procedures may be performed to repair the aneurysm and prevent re-bleeding.
Prompt recognition and treatment of subarachnoid hemorrhage are crucial to minimize neurological damage and improve outcomes. Even with appropriate treatment, subarachnoid hemorrhage can be a life-threatening condition associated with significant morbidity and mortality, so early intervention is essential.
The Heart
01.Myocardial infarct due to coronary thrombosis(Images obtained from the Department of pathology, Faculty of Medicine, University of Kelaniya)
Myocardial infarction (MI), commonly known as a heart attack, occurs when there is a sudden blockage of blood flow to a part of the heart muscle. This blockage is often caused by a blood clot (thrombosis) forming in one of the coronary arteries, which are responsible for supplying oxygen-rich blood to the heart muscle.
Cause:
Coronary Thrombosis: The most common cause of myocardial infarction is the formation of a blood clot (thrombus) within one of the coronary arteries. This clot can block blood flow, leading to ischemia (lack of oxygen) and damage to the heart muscle.
Symptoms:
Chest Pain: Typically described as a crushing or squeezing sensation in the center or left side of the chest. The pain may radiate to the arm, neck, jaw, back, or stomach.
Shortness of Breath: Difficulty breathing, especially with exertion or at rest.
Nausea and Vomiting: Some people may experience these symptoms, along with lightheadedness or dizziness.
Sweating: Profuse sweating, often accompanied by a feeling of impending doom.
Irregular Heartbeat: Palpitations or a feeling of the heart skipping beats.
Diagnosis:
- Electrocardiogram (ECG or EKG): This test records the electrical activity of the heart and can detect abnormalities indicative of myocardial infarction, such as ST-segment elevation.
- Blood Tests: Measurement of cardiac enzymes (troponin, creatine kinase-MB) released into the bloodstream when heart muscle cells are damaged.
- Imaging Tests: Echocardiogram, cardiac MRI, or coronary angiography may be performed to assess heart function and visualize the coronary arteries for blockages.
Treatment:
Medications:
- Thrombolytics: Drugs like tissue plasminogen activator (tPA) may be administered to dissolve the blood clot and restore blood flow.
- Antiplatelet Drugs: Aspirin and clopidogrel help prevent further clot formation.
- Pain Relief: Nitroglycerin may be given to relieve chest pain.
- Beta-blockers and ACE Inhibitors: To reduce the workload on the heart and improve its function.
Percutaneous Coronary Intervention (PCI): Also known as angioplasty, this procedure involves inserting a catheter with a balloon at its tip into the blocked artery to widen it and often placing a stent to keep it open.
Coronary Artery Bypass Grafting (CABG): In cases where PCI is not feasible or effective, surgery may be performed to bypass the blocked artery using a graft.
Rehabilitation:
Cardiac Rehabilitation: This program involves exercise training, education, and counseling to help patients recover from a heart attack and reduce the risk of future cardiac events.
Lifestyle Changes: Quitting smoking, adopting a heart-healthy diet, maintaining a healthy weight, and managing conditions like high blood pressure and diabetes are essential for long-term heart health.
Immediate medical attention is crucial for anyone experiencing symptoms suggestive of a heart attack. Prompt treatment can minimize damage to the heart muscle and improve outcomes.
02.Recent myocardial infarct
Recent myocardial infarction (MI), also known as an acute heart attack, refers to a heart attack that has occurred within a short time frame, usually within the past few days or weeks.
Causes:
- Coronary Artery Disease (CAD): The primary cause of myocardial infarction is the buildup of plaque within the coronary arteries, leading to atherosclerosis.
- Coronary Thrombosis: Acute plaque rupture or erosion can trigger the formation of a blood clot (thrombus) within a coronary artery, leading to sudden blockage of blood flow.
- Spasm of Coronary Arteries: In some cases, the coronary arteries may undergo spasms, leading to a temporary reduction or cessation of blood flow to a part of the heart muscle.
Symptoms:
- Chest Pain: Typically described as a crushing, squeezing, or pressure-like sensation in the center or left side of the chest. The pain may radiate to the arm, neck, jaw, back, or stomach.
- Shortness of Breath: Difficulty breathing, especially with exertion or at rest.
- Nausea and Vomiting: Some individuals may experience these symptoms, along with lightheadedness or dizziness.
- Sweating: Profuse sweating, often accompanied by a feeling of impending doom.
- Irregular Heartbeat: Palpitations or a sensation of the heart skipping beats.
Diagnosis:
- Electrocardiogram (ECG or EKG): This test records the electrical activity of the heart and can detect abnormalities indicative of a recent myocardial infarction, such as ST-segment elevation or depression, T-wave changes, or the presence of Q waves.
- Blood Tests: Measurement of cardiac biomarkers such as troponin, creatine kinase-MB, and myoglobin, which are released into the bloodstream when heart muscle cells are damaged.
- Imaging Tests: Echocardiogram, cardiac MRI, or coronary angiography may be performed to assess heart function and visualize the coronary arteries for blockages.
Treatment:
- Antiplatelet Drugs: Aspirin, clopidogrel, or other antiplatelet medications to prevent further blood clot formation.
- Thrombolytics: If the patient presents early and primary percutaneous coronary intervention (PCI) is not immediately available, thrombolytic therapy may be administered to dissolve the blood clot and restore blood flow.
- Pain Relief: Nitroglycerin or other medications to alleviate chest pain.
- Beta-blockers, ACE Inhibitors, and Statins: To improve heart function, reduce blood pressure, and lower cholesterol levels, respectively.
- Reperfusion Therapy: Primary PCI is the preferred method of reperfusion if it can be performed promptly and safely. This involves mechanically opening the blocked coronary artery with angioplasty and stent placement.
- Coronary Artery Bypass Grafting (CABG): In cases where PCI is not feasible or effective, bypass surgery may be considered to restore blood flow to the heart muscle.
- Cardiac Rehabilitation: After stabilization, participation in a cardiac rehabilitation program is recommended to promote recovery, improve cardiovascular fitness, and reduce the risk of future cardiac events.
Prompt recognition and treatment of a recent myocardial infarction are essential to minimize damage to the heart muscle and improve outcomes. Individuals who experience symptoms suggestive of a heart attack should seek immediate medical attention.
03.Aortic stenosis with left ventricular hypertrophy
(Images obtained from the Department of pathology, Faculty of Medicine, University of Kelaniya)
Aortic stenosis with left ventricular hypertrophy is a condition characterized by narrowing (stenosis) of the aortic valve, which obstructs blood flow from the left ventricle of the heart to the aorta. This obstruction leads to increased pressure within the left ventricle, causing it to become thickened and enlarged, a condition known as left ventricular hypertrophy (LVH).
Degenerative Valve Disease: Aortic stenosis is often caused by age-related degeneration and calcification of the aortic valve.Congenital Malformations: Some individuals may be born with abnormalities of the aortic valve, leading to stenosis.Rheumatic Fever: In regions where rheumatic fever is prevalent, scarring and thickening of the aortic valve may occur, causing stenosis.Bicuspid Aortic Valve: Individuals born with a bicuspid rather than a tricuspid aortic valve are at increased risk of developing aortic stenosis.
Symptoms:- Chest Pain: Angina or chest discomfort, especially during physical exertion.
- Shortness of Breath: Dyspnea, particularly with exertion or when lying flat (orthopnea).
- Fatigue: Weakness or tiredness, often due to reduced cardiac output.
- Dizziness or Syncope: Fainting spells or near-fainting episodes may occur due to reduced blood flow to the brain.
- Heart Murmur: A characteristic heart murmur, often described as a harsh, crescendo-decrescendo sound, may be audible upon auscultation.
Diagnosis:- Physical Examination: A healthcare provider may detect signs of aortic stenosis, such as a heart murmur or abnormal pulse.
- Echocardiography: This imaging test provides detailed images of the heart and can assess the severity of aortic stenosis, as well as detect left ventricular hypertrophy.
- Electrocardiogram (ECG or EKG): This test records the electrical activity of the heart and may show signs of LVH, such as widened QRS complexes or ST-T wave changes.
- Cardiac Catheterization: Invasive testing to directly measure pressures within the heart and assess coronary artery anatomy, which may be necessary before certain interventions.
Treatments:
- Vasodilators: Drugs such as ACE inhibitors or angiotensin receptor blockers (ARBs) may help reduce symptoms and delay disease progression.
- Diuretics: To alleviate symptoms of fluid retention and congestion.
- Beta-blockers: These medications can help reduce heart rate and improve symptoms.
- Aortic Valve Replacement (AVR): This is the definitive treatment for severe symptomatic aortic stenosis. It may involve surgical replacement of the valve with a mechanical or bioprosthetic valve or transcatheter aortic valve replacement (TAVR) for selected patients.
- Monitoring: Regular follow-up with a cardiologist is essential to monitor disease progression and adjust treatment as needed.
- Lifestyle Modifications: Patients are often advised to adopt heart-healthy habits, including regular exercise, smoking cessation, and a balanced diet low in sodium and saturated fats.
Early detection and appropriate management of aortic stenosis with left ventricular hypertrophy are crucial for improving outcomes and quality of life. Patients experiencing symptoms suggestive of aortic stenosis should seek evaluation by a healthcare provider.
Aortic stenosis with left ventricular hypertrophy is a condition characterized by narrowing (stenosis) of the aortic valve, which obstructs blood flow from the left ventricle of the heart to the aorta. This obstruction leads to increased pressure within the left ventricle, causing it to become thickened and enlarged, a condition known as left ventricular hypertrophy (LVH).
Degenerative Valve Disease: Aortic stenosis is often caused by age-related degeneration and calcification of the aortic valve.
Congenital Malformations: Some individuals may be born with abnormalities of the aortic valve, leading to stenosis.
Rheumatic Fever: In regions where rheumatic fever is prevalent, scarring and thickening of the aortic valve may occur, causing stenosis.
Bicuspid Aortic Valve: Individuals born with a bicuspid rather than a tricuspid aortic valve are at increased risk of developing aortic stenosis.
Symptoms:
- Chest Pain: Angina or chest discomfort, especially during physical exertion.
- Shortness of Breath: Dyspnea, particularly with exertion or when lying flat (orthopnea).
- Fatigue: Weakness or tiredness, often due to reduced cardiac output.
- Dizziness or Syncope: Fainting spells or near-fainting episodes may occur due to reduced blood flow to the brain.
- Heart Murmur: A characteristic heart murmur, often described as a harsh, crescendo-decrescendo sound, may be audible upon auscultation.
Diagnosis:
- Physical Examination: A healthcare provider may detect signs of aortic stenosis, such as a heart murmur or abnormal pulse.
- Echocardiography: This imaging test provides detailed images of the heart and can assess the severity of aortic stenosis, as well as detect left ventricular hypertrophy.
- Electrocardiogram (ECG or EKG): This test records the electrical activity of the heart and may show signs of LVH, such as widened QRS complexes or ST-T wave changes.
- Cardiac Catheterization: Invasive testing to directly measure pressures within the heart and assess coronary artery anatomy, which may be necessary before certain interventions.
Treatments:
- Vasodilators: Drugs such as ACE inhibitors or angiotensin receptor blockers (ARBs) may help reduce symptoms and delay disease progression.
- Diuretics: To alleviate symptoms of fluid retention and congestion.
- Beta-blockers: These medications can help reduce heart rate and improve symptoms.
- Aortic Valve Replacement (AVR): This is the definitive treatment for severe symptomatic aortic stenosis. It may involve surgical replacement of the valve with a mechanical or bioprosthetic valve or transcatheter aortic valve replacement (TAVR) for selected patients.
- Monitoring: Regular follow-up with a cardiologist is essential to monitor disease progression and adjust treatment as needed.
- Lifestyle Modifications: Patients are often advised to adopt heart-healthy habits, including regular exercise, smoking cessation, and a balanced diet low in sodium and saturated fats.
Early detection and appropriate management of aortic stenosis with left ventricular hypertrophy are crucial for improving outcomes and quality of life. Patients experiencing symptoms suggestive of aortic stenosis should seek evaluation by a healthcare provider.
04.Left ventricular hypertrophy
Left ventricular hypertrophy (LVH) is the thickening of the muscular wall of the heart's left ventricle, often caused by conditions such as hypertension, aortic stenosis, or hypertrophic cardiomyopathy. While LVH can be asymptomatic, symptoms may include chest pain, shortness of breath, fatigue, and palpitations. Treatment involves managing underlying conditions, medications to lower blood pressure and control symptoms, lifestyle modifications, regular monitoring, and sometimes surgical intervention or implantable devices in severe cases.
05.Mitral stenosis
(Images obtained from the Department of pathology, Faculty of Medicine, University of Kelaniya)
Mitral stenosis is a narrowing of the mitral valve opening in the heart, commonly caused by rheumatic fever. Symptoms include shortness of breath, fatigue, palpitations, and difficulty lying flat. Treatment may involve medications to manage symptoms, procedures like balloon valvuloplasty to open the valve, or surgical repair or replacement. Lifestyle changes and regular monitoring are also important aspects of management.
The Lung
01.Lung Tumor
(Images obtained from the Department of pathology, Faculty of Medicine, University of Kelaniya)
A lung tumor refers to an abnormal growth of cells within the lung tissue. There are two main types of lung tumors: benign tumors, which are non-cancerous, and malignant tumors, which are cancerous. Malignant tumors are further categorized into two main types: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC).
Causes:
- Smoking: Tobacco smoking is the leading cause of lung cancer. It accounts for the majority of lung cancer cases worldwide.
- Secondhand smoke: Exposure to secondhand smoke also increases the risk of developing lung cancer.
- Occupational exposure: Exposure to carcinogens such as asbestos, radon, arsenic, and certain chemicals can increase the risk of lung cancer.
- Genetics: Some genetic factors may predispose individuals to lung cancer, although this is less common.
Symptoms:
- Persistent cough: A cough that doesn't go away or worsens over time.
- Chest pain: Pain in the chest, shoulder, or back that worsens with deep breathing, coughing, or laughing.
- Shortness of breath: Difficulty breathing, wheezing, or hoarseness.
- Unexplained weight loss: Significant and unexplained weight loss.
- Coughing up blood: Blood in the sputum or phlegm.
- Fatigue: Feeling tired or weak.
- Loss of appetite: Reduced appetite or changes in eating habits.
- Recurring respiratory infections: Such as bronchitis or pneumonia.
Diagnosis:
- Imaging tests: Chest X-ray, CT scan, or MRI to visualize the lung and detect any abnormalities.
- Biopsy: Removal of a sample of lung tissue for examination under a microscope to determine if it's cancerous.
- Sputum cytology: Examination of sputum (mucus coughed up from the lungs) under a microscope to check for cancer cells.
- Bronchoscopy: A procedure in which a thin, flexible tube with a camera is passed through the mouth or nose into the lungs to view the airways and collect tissue samples.
- PET scan: A scan that uses a radioactive tracer to highlight areas of cancer cells in the body.
Treatment:
- Surgery: Surgical removal of the tumor and surrounding tissue, particularly in the early stages of lung cancer.
- Chemotherapy: The use of drugs to kill cancer cells or stop them from growing.
- Radiation therapy: The use of high-energy radiation to kill cancer cells or shrink tumors.
- Targeted therapy: Drugs that target specific abnormalities present within cancer cells, such as genetic mutations.
- Immunotherapy: Treatment that helps the immune system fight cancer by stimulating the body's natural defenses
02.Adenoma of bronchus
(Images obtained from the Department of pathology, Faculty of Medicine, University of Kelaniya)
Adenoma of the bronchus is a benign tumor that originates from the epithelial lining of the bronchial tubes in the lungs. These tumors typically grow slowly and are non-cancerous, meaning they do not spread to other parts of the body. Adenomas of the bronchus are relatively rare compared to malignant lung tumors, such as lung cancer.
Symptoms of bronchial adenoma may include persistent coughing, wheezing, shortness of breath, chest pain, coughing up blood (hemoptysis), and recurrent respiratory infections. However, in some cases, these tumors may be asymptomatic and discovered incidentally during medical imaging or procedures for other conditions.
Diagnosis of bronchial adenoma typically involves imaging studies such as chest X-rays, CT scans, or MRI scans to visualize the tumor, as well as bronchoscopy to obtain tissue samples for biopsy. Treatment options for bronchial adenoma may include surgical removal of the tumor, endoscopic techniques to remove or shrink the tumor, or other interventions depending on the size, location, and symptoms associated with the tumor.
While adenomas of the bronchus are generally benign, they can still cause significant symptoms and complications if left untreated. Therefore, prompt diagnosis and appropriate management are important to prevent complications and improve the patient's quality of life.
03.Carcinoma of lung
(Images obtained from the Department of pathology, Faculty of Medicine, University of Kelaniya)
Lung carcinoma, commonly referred to as lung cancer, is a malignant tumor that arises from the cells lining the air passages within the lungs. It is one of the most prevalent and deadliest forms of cancer worldwide, primarily attributed to tobacco smoking but also influenced by environmental factors and genetic predispositions. Lung carcinomas are broadly categorized into two main types: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC), each with distinct characteristics and treatment approaches. Symptoms of lung carcinoma may include persistent cough, chest pain, shortness of breath, coughing up blood, weight loss, and fatigue. Diagnosis typically involves imaging studies, such as chest X-rays and CT scans, along with biopsy for confirmation. Treatment options depend on the type and stage of lung cancer but may include surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy. Prognosis varies widely depending on factors such as the stage of the cancer at diagnosis, overall health, and response to treatment, emphasizing the importance of early detection and comprehensive management strategies.
04.Pneumonia
(Images obtained from the Department of pathology, Faculty of Medicine, University of Kelaniya)
Pneumonia is an infection that inflames the air sacs in one or both lungs, causing them to fill with fluid or pus. It can be caused by a variety of infectious agents, including bacteria, viruses, and fungi.
Causes:
- Bacteria: The most common bacterial cause of pneumonia is Streptococcus pneumoniae. Other bacteria, such as Hemophilus influenzae and Mycoplasma pneumoniae, can also cause pneumonia.
- Viruses: Influenza viruses, respiratory syncytial virus (RSV), and adenoviruses are common viral causes of pneumonia, especially in children and the elderly.
- Fungi: Fungal pneumonia is less common but can occur in people with weakened immune systems, such as those with HIV/AIDS or undergoing chemotherapy.
- Aspiration: Inhaling food, liquids, saliva, or vomit into the lungs can cause a type of pneumonia called aspiration pneumonia.
Symptoms:
- Cough: Often producing phlegm (sputum) that may be green, yellow, or bloody.
- Fever: Sometimes high fever with shaking chills.
- Difficulty breathing: Shortness of breath, rapid breathing, or chest pain when breathing deeply.
- Fatigue: Feeling unusually tired or weak.
- Nausea, vomiting, or diarrhea: Especially in children.
- Confusion or changes in mental awareness: Especially in older adults.
Diagnosis:
- Physical examination: A doctor will listen to the lungs with a stethoscope for abnormal breath sounds, such as crackling or wheezing.
- Chest X-ray: To visualize the lungs and identify areas of inflammation or fluid buildup.
- Blood tests: To check for signs of infection, such as elevated white blood cell count.
- Sputum culture: A sample of mucus may be collected and analyzed to identify the specific organism causing the infection.
Treatment:
- Antibiotics: If the pneumonia is caused by bacteria, antibiotics are prescribed. The choice of antibiotic depends on the type of bacteria suspected and other factors such as the patient's age and overall health.
- Antiviral medications: If the pneumonia is caused by a virus, antiviral medications may be prescribed. However, viral pneumonia often resolves on its own with supportive care.
- Antifungal medications: For fungal pneumonia, antifungal medications are prescribed.
- Supportive care: This may include rest, staying hydrated, and using over-the-counter pain relievers and fever reducers.
- Oxygen therapy: If oxygen levels are low, supplemental oxygen may be provided through nasal prongs or a mask.
- Hospitalization: Severe cases of pneumonia, especially in young children, older adults, or those with underlying health conditions, may require hospitalization for intravenous antibiotics, oxygen therapy, and close monitoring.
In summary, pneumonia is a common and potentially serious infection of the lungs that requires prompt diagnosis and appropriate treatment to prevent complications and promote recovery. Vaccines, such as the pneumococcal vaccine and the flu vaccine, can help prevent some types of pneumonia.
The Stomach
01.Perforated peptic ulcer
(Images obtained from the Department of pathology, Faculty of Medicine, University of Kelaniya)
A perforated peptic ulcer occurs when an ulcer in the stomach, small intestine, or esophagus erodes completely through the wall, leading to a hole that allows the contents of the digestive tract to leak into the abdominal cavity.
Helicobacter pylori infection: This bacterium can weaken the protective lining of the stomach and intestines, making them more susceptible to ulcers.Nonsteroidal anti-inflammatory drugs (NSAIDs): Prolonged use of medications like aspirin, ibuprofen, or naproxen can increase the risk of peptic ulcers.Excessive alcohol consumption: Alcohol can irritate the stomach lining and increase the risk of ulcer formation.Smoking: Tobacco use can interfere with the healing of ulcers and increase the risk of complications.Stress: While stress doesn't directly cause ulcers, it can worsen symptoms and delay healing.
Symptoms:- Sudden, severe abdominal pain: Often located in the upper abdomen, which may radiate to the back or shoulders.
- Tenderness: The abdomen may be tender to the touch.
- Nausea and vomiting: Sometimes accompanied by vomiting blood.
- Bloating and abdominal distention: Due to the leakage of digestive juices into the abdominal cavity.
- Fever and chills: Signs of infection may be present if the perforation leads to peritonitis (inflammation of the abdominal cavity).
Diagnosis:
- Physical examination: A doctor may perform a physical exam to assess symptoms and signs of peritonitis.
- Imaging tests: X-rays or CT scans can help visualize air or fluid in the abdominal cavity, indicating a perforation.
- Endoscopy: A thin, flexible tube with a camera (endoscope) may be inserted through the mouth to examine the digestive tract and identify the ulcer.
- Blood tests: Tests for anemia or signs of infection may be performed.
Treatment:
- Surgery: Emergency surgery is usually necessary to repair the perforation and remove any infected tissue.
- Antibiotics: To treat any underlying infection, particularly if peritonitis is present.
- Proton pump inhibitors (PPIs) or H2-receptor antagonists: These medications reduce stomach acid production and promote ulcer healing.
- Intravenous fluids and electrolytes: To maintain hydration and replace lost fluids.
- Pain management: Pain medications may be administered to alleviate discomfort.
Prompt diagnosis and treatment are crucial in cases of perforated peptic ulcers to prevent serious complications such as peritonitis, sepsis, and organ failure. After treatment, lifestyle modifications such as avoiding NSAIDs, reducing stress, and quitting smoking may help prevent recurrence.
A perforated peptic ulcer occurs when an ulcer in the stomach, small intestine, or esophagus erodes completely through the wall, leading to a hole that allows the contents of the digestive tract to leak into the abdominal cavity.
Helicobacter pylori infection: This bacterium can weaken the protective lining of the stomach and intestines, making them more susceptible to ulcers.
Nonsteroidal anti-inflammatory drugs (NSAIDs): Prolonged use of medications like aspirin, ibuprofen, or naproxen can increase the risk of peptic ulcers.
Excessive alcohol consumption: Alcohol can irritate the stomach lining and increase the risk of ulcer formation.
Smoking: Tobacco use can interfere with the healing of ulcers and increase the risk of complications.
Stress: While stress doesn't directly cause ulcers, it can worsen symptoms and delay healing.
Symptoms:
- Sudden, severe abdominal pain: Often located in the upper abdomen, which may radiate to the back or shoulders.
- Tenderness: The abdomen may be tender to the touch.
- Nausea and vomiting: Sometimes accompanied by vomiting blood.
- Bloating and abdominal distention: Due to the leakage of digestive juices into the abdominal cavity.
- Fever and chills: Signs of infection may be present if the perforation leads to peritonitis (inflammation of the abdominal cavity).
Diagnosis:
- Physical examination: A doctor may perform a physical exam to assess symptoms and signs of peritonitis.
- Imaging tests: X-rays or CT scans can help visualize air or fluid in the abdominal cavity, indicating a perforation.
- Endoscopy: A thin, flexible tube with a camera (endoscope) may be inserted through the mouth to examine the digestive tract and identify the ulcer.
- Blood tests: Tests for anemia or signs of infection may be performed.
Treatment:
- Surgery: Emergency surgery is usually necessary to repair the perforation and remove any infected tissue.
- Antibiotics: To treat any underlying infection, particularly if peritonitis is present.
- Proton pump inhibitors (PPIs) or H2-receptor antagonists: These medications reduce stomach acid production and promote ulcer healing.
- Intravenous fluids and electrolytes: To maintain hydration and replace lost fluids.
- Pain management: Pain medications may be administered to alleviate discomfort.
Prompt diagnosis and treatment are crucial in cases of perforated peptic ulcers to prevent serious complications such as peritonitis, sepsis, and organ failure. After treatment, lifestyle modifications such as avoiding NSAIDs, reducing stress, and quitting smoking may help prevent recurrence.
02.Diffuse Gastric Carcinoma- Leather Bottle Stomach
(Images obtained from the Department of pathology, Faculty of Medicine, University of Kelaniya)
Diffuse gastric carcinoma, also known as leather bottle stomach or linitis plastica, is a rare and aggressive form of stomach cancer characterized by the thickening and stiffening of the stomach wall.
Causes:
- Genetic factors: Certain genetic mutations, such as mutations in the CDH1 gene, are associated with an increased risk of diffuse gastric carcinoma, particularly in families with a history of hereditary diffuse gastric cancer syndrome.
- Helicobacter pylori infection: Chronic infection with H. pylori, a bacterium that infects the stomach lining, is a risk factor for developing stomach cancer, including diffuse gastric carcinoma.
- Dietary factors: Consuming a diet high in smoked, pickled, or salted foods, as well as low intake of fruits and vegetables, may increase the risk of stomach cancer.
- Environmental factors: Exposure to certain environmental toxins or pollutants may contribute to the development of gastric cancer.
Symptoms:
- Early satiety: Feeling full after eating a small amount of food.
- Persistent indigestion or heartburn: Especially if it doesn't improve with over-the-counter medications.
- Unexplained weight loss: Significant and unintentional weight loss over a short period.
- Abdominal pain or discomfort: Pain or discomfort in the abdomen, particularly in the upper abdomen.
- Nausea and vomiting: Especially if it persists or worsens over time.
- Difficulty swallowing (dysphagia): Due to narrowing of the stomach or esophagus.
- Fatigue: Feeling tired or weak, often due to anemia caused by bleeding from the tumor.
Diagnosis:
- Endoscopy: A thin, flexible tube with a camera (endoscope) is inserted through the mouth and into the stomach to visualize the lining and obtain biopsy samples.
- Biopsy: Tissue samples obtained during endoscopy are examined under a microscope to confirm the presence of cancer cells.
- Imaging tests: CT scans, PET scans, or MRI scans may be performed to evaluate the extent of the cancer and identify any spread to nearby organs or lymph nodes.
Treatment:
- Surgery: Surgical removal of the tumor and surrounding tissue (partial or total gastrectomy) is the primary treatment for diffuse gastric carcinoma, if feasible.
- Chemotherapy: Chemotherapy may be used before surgery (neoadjuvant chemotherapy) to shrink the tumor and make it easier to remove, or after surgery (adjuvant chemotherapy) to kill any remaining cancer cells and reduce the risk of recurrence.
- Radiation therapy: Radiation therapy may be used in combination with surgery or chemotherapy to kill cancer cells and shrink tumors.
- Targeted therapy: Drugs that target specific abnormalities present within cancer cells, such as HER2 inhibitors, may be used in cases where the tumor overexpresses certain proteins or genes.
- Palliative care: In cases where the cancer is advanced and cannot be cured, palliative care focuses on relieving symptoms, improving quality of life, and providing emotional support.
Overall, the prognosis for diffuse gastric carcinoma is often poor due to its aggressive nature and tendency to spread rapidly. However, early detection and aggressive treatment can improve outcomes and quality of life for some patients.
(Images obtained from the Department of pathology, Faculty of Medicine, University of Kelaniya)
Diffuse gastric carcinoma, also known as leather bottle stomach or linitis plastica, is a rare and aggressive form of stomach cancer characterized by the thickening and stiffening of the stomach wall.
Causes:
- Genetic factors: Certain genetic mutations, such as mutations in the CDH1 gene, are associated with an increased risk of diffuse gastric carcinoma, particularly in families with a history of hereditary diffuse gastric cancer syndrome.
- Helicobacter pylori infection: Chronic infection with H. pylori, a bacterium that infects the stomach lining, is a risk factor for developing stomach cancer, including diffuse gastric carcinoma.
- Dietary factors: Consuming a diet high in smoked, pickled, or salted foods, as well as low intake of fruits and vegetables, may increase the risk of stomach cancer.
- Environmental factors: Exposure to certain environmental toxins or pollutants may contribute to the development of gastric cancer.
Symptoms:
- Early satiety: Feeling full after eating a small amount of food.
- Persistent indigestion or heartburn: Especially if it doesn't improve with over-the-counter medications.
- Unexplained weight loss: Significant and unintentional weight loss over a short period.
- Abdominal pain or discomfort: Pain or discomfort in the abdomen, particularly in the upper abdomen.
- Nausea and vomiting: Especially if it persists or worsens over time.
- Difficulty swallowing (dysphagia): Due to narrowing of the stomach or esophagus.
- Fatigue: Feeling tired or weak, often due to anemia caused by bleeding from the tumor.
Diagnosis:
- Endoscopy: A thin, flexible tube with a camera (endoscope) is inserted through the mouth and into the stomach to visualize the lining and obtain biopsy samples.
- Biopsy: Tissue samples obtained during endoscopy are examined under a microscope to confirm the presence of cancer cells.
- Imaging tests: CT scans, PET scans, or MRI scans may be performed to evaluate the extent of the cancer and identify any spread to nearby organs or lymph nodes.
Treatment:
- Surgery: Surgical removal of the tumor and surrounding tissue (partial or total gastrectomy) is the primary treatment for diffuse gastric carcinoma, if feasible.
- Chemotherapy: Chemotherapy may be used before surgery (neoadjuvant chemotherapy) to shrink the tumor and make it easier to remove, or after surgery (adjuvant chemotherapy) to kill any remaining cancer cells and reduce the risk of recurrence.
- Radiation therapy: Radiation therapy may be used in combination with surgery or chemotherapy to kill cancer cells and shrink tumors.
- Targeted therapy: Drugs that target specific abnormalities present within cancer cells, such as HER2 inhibitors, may be used in cases where the tumor overexpresses certain proteins or genes.
- Palliative care: In cases where the cancer is advanced and cannot be cured, palliative care focuses on relieving symptoms, improving quality of life, and providing emotional support.
Overall, the prognosis for diffuse gastric carcinoma is often poor due to its aggressive nature and tendency to spread rapidly. However, early detection and aggressive treatment can improve outcomes and quality of life for some patients.
The Liver
01.Macromoduler cirrhosis
(Images obtained from the Department of pathology, Faculty of Medicine, University of Kelaniya)
Macronodular cirrhosis is a type of liver cirrhosis characterized by the presence of large, visible nodules or masses in the liver tissue. These nodules are typically greater than 3 millimeters in size and are surrounded by fibrous tissue. Macronodular cirrhosis is often a result of chronic liver damage and inflammation, such as that caused by long-term alcohol abuse, chronic hepatitis B or C infection, autoimmune hepatitis, or non-alcoholic fatty liver disease. As the condition progresses, the liver becomes increasingly scarred and dysfunctional, leading to complications such as portal hypertension, ascites (fluid buildup in the abdomen), hepatic encephalopathy (brain dysfunction due to liver failure), and an increased risk of liver cancer. Treatment aims to manage symptoms, slow disease progression, and address underlying causes, which may include lifestyle changes, medications, and in some cases, liver transplantation. Early diagnosis and intervention are crucial in managing macronodular cirrhosis and improving outcomes for affected individuals.
02.Biliary cirrhosis
Biliary cirrhosis, also known as primary biliary cirrhosis (PBC), is a chronic liver disease characterized by progressive inflammation and destruction of the small bile ducts within the liver. This condition primarily affects middle-aged women and is believed to result from an autoimmune reaction, whereby the body's immune system mistakenly attacks the bile ducts. Over time, the damage to the bile ducts leads to impaired bile flow, accumulation of bile within the liver, and subsequent liver scarring or cirrhosis. Symptoms of biliary cirrhosis may include fatigue, itching, dry eyes, dry mouth, abdominal pain, and jaundice. If left untreated, biliary cirrhosis can progress to liver failure and complications such as portal hypertension, ascites, and hepatic encephalopathy. Treatment for biliary cirrhosis aims to manage symptoms, slow disease progression, and improve liver function through medications such as ursodeoxycholic acid (UDCA), which helps promote bile flow, as well as liver transplantation in advanced cases. Early diagnosis and intervention are crucial in managing biliary cirrhosis and improving long-term outcomes.
References:
- What are the 4 stages of cirrhosis? (no date). Available at: https://medlicker.com/934-four-stages-of-cirrhosis.
- Waugh, A. and Grant, A. (2014) Ross and Wilson Anatomy and Physiology in health and illness. 12th edn. United Kingdom: Elsevier.
- Editorial (2019) Pneumonia: Symptoms and treatment of pneumonia, Doc said. Available at: https://doc-said.com/articles/diseases/pneumonia-symptoms-and-treatment/
- Akbar, H. et al. (2023) Acute ST-Elevation myocardial infarction. Available at: https://www.ncbi.nlm.nih.gov/books/NBK532281/.
- Nelson, J.R. et al. (2017) ‘Potential benefits of eicosapentaenoic acid on atherosclerotic plaques’, Vascular Pharmacology, 91, pp. 1–9.Available at: https://doi.org/10.1016/j.vph.2017.02.004.

















Comments
Post a Comment